I was recently with a client of mine who also happens to be a friend. While we were waiting for her baby to finish breastfeeding we were chatting and catching up. When conversation turned to my recent crazy breastfeeding experiences I found myself having a hard time coming up with a cliff notes version.
Our issues were layered.
They got worse before they got better.
They got better slowly.
It started out so normal. At first everything seemed to be relatively smooth sailing. My birth was very fast and intense but also powerful and healing. I had the intervention free natural birth that I had always hoped for. He breastfed right away and within five hours of his first time in my arms I was home in bed with my husband and son. We spent our time skin to skin, snuggling, watching movies with my older kids, and feeding on demand.
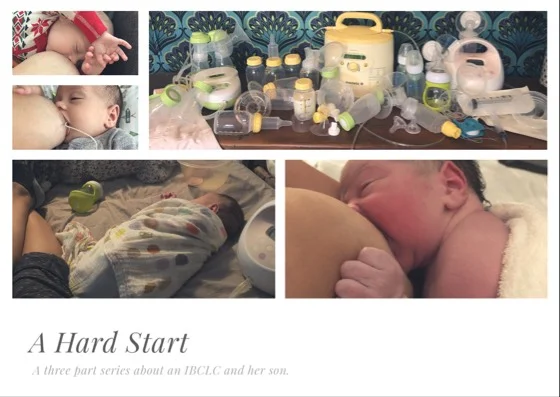
Image by Rachael Anastasio Collins
I wasn’t alarmed about the tongue and lip ties that I saw. I was expecting them after my experiences with my other kids. I saw them as a minor inconvenience that I would just take care of and move on. My latch was a tad uncomfortable but not terrible and he was happy and growing. I also noticed pretty early on that he kept his head turned to one side with even his gaze was stuck with his sweet eyes looking mostly in one direction. This congenital torticollis didn’t surprise me that much either. I frequently commented during my pregnancy that he stayed in the same spot all the time, he kicked around but never really rolled side to side.
I figured it wouldn’t be a huge deal. I am a professional, after all. I did the things I know to do. I made the appointments I needed to make and expected things to go according to plan. A wonderful friend of mine happens to be a pretty fabulous chiropractor and she gifted us with a meal and an adjustment for my guy soon after his birth. I made an appointment with a Craniosacral Therapist that I respect in town. I planned to start bodywork and then make an appointment for his lip and tongue tie release. I had it covered.
At three weeks old his lip and tongue ties were released by a great provider in my town and my boy handled the procedure surprisingly well. I did my aftercare, nursed my baby, and took him to his appointments with a physical therapist and then an occupational therapist to tackle the torticollis.
Do the things. It will be good.
But, it wasn’t.
He wanted to feed constantly but would quickly fall asleep at the breast. Every time I would go to move him he would root around hungrily and cry, latch back on, suck a little, and then fall asleep again. This was not simply cluster feeding. This was all day long. His weight gain each week kept slowing and there was a period of a few days where he didn’t poop at all. I started to get more and more concerned. I kept doing all the right things—aftercare, sucking exercises, physical therapy, occupational therapy, CST, and chiro—but it was getting worse. He seemed to become more lethargic at the breast, sucking weakly and ineffectively. His tongue was not moving correctly. It was just bunching in the back of his mouth. For some reason, I decided to dig out my stethoscope and listen to his heartbeat. There was a heart murmur. Something that isn’t all that strange in a new baby but my panicked mind was connecting random dots thinking that maybe he had a heart defect causing him to feed poorly. Cue anxiety overload and a call to our pediatrician. An echocardiogram ruled out that worry when it confirmed that the murmur (small pat on the back for still having those nurse assessment skills) was actually caused by two small holes that will most likely close without issues but that wouldn’t contribute to feeding problems or cause fatigue in my boy.
What the hell was going on? The more his tensions unwound the more he seemed to fall apart. What kind of horrible lactation consultant was I that I was struggling to fix him?
I called up an IBCLC friend of mine just to see if she was seeing what I was seeing. She did and cofirmed what I was thinking — he needed more to eat because he wasn’t able to pull enough milk from my breasts on his own. I had to start supplementing with my expressed milk.
I started pumping to increase my supply because it was wrecked after weeks of sub par nursing. He was so ineffective at pulling milk from my breasts that my supply started drying up. My mom came into town and my husband worked from home one day so that I could get it back. I rented a hospital-grade pump and for four days I pumped 10-12 times a day in addition to breastfeeding and supplementing my baby with my milk. I filled my freezer with 60 ounces of breastmilk donated from a friend because I wasn’t producing a full supply.
Image by Rachael Anastasio Collins
My professional brain was trying to do its job while my tired, emotional, and freshly postpartum mom brain was going crazy. Finally I waved the white flag and called a colleague. I surrendered to her expertise and treatment plans. My IBCLC hat came off and I embraced being the mom. I told her to just tell me what to do and I would do it.
I got to experience the other side of the relationship that I form with people in the course of my work.
She assessed, helped, made suggestions and treatment plans. She supported and encouraged and taught me new tricks. She answered my texts and calls. Many, many calls. She made gentle suggestions and supported me. She made firm suggestions and bolstered me. She collaborated with others to find the best tools for my silly baby boy who hated some of our typical devices. I followed instructions and did the work.
I triple fed my baby for weeks where I would put him to the breast first, then feeding him expressed milk from different devices, and finally I would pump to protect my supply and collect the milk he would eat later. We tried every breastfeeding aid and tool we could think of— different bottles, different techniques, different exercises, so much patience, different pumps and types of flanges to find the most comfortable fit, craniosacral therapy, craniofascial therapy, chiropractic treatment, physical therapy, occupational therapy, a second trip to the pediatric dentist for a buccal tie release, rebirthing in the tub, supplemental nursing systems, special needs feeders, tubes, and syringes. My husband and I washed pump parts constantly. I started an SSRI to treat my postpartum anxiety that was not being helped by the feeding struggles.
All of the equipment we used on our journey to successful breastfeeding. Image by Rachael Anastasio Collins.
I cried a lot. I smiled too. I remember one particular moment when I was going through the motions of bottle feeding and happened to look down at my boy who locked eyes with me and gave me a gummy grin. It was like he was telling me that even through all of the crap we were going through that he was happy and loved me and we were in it together. I messaged with friends that had hard starts too, received a beautiful note of encouragement from my mother in law, a hilarious card from my cousin that made me laugh and served as a reminder to keep going, and made daily calls to my own mother. I spent my time rocking my baby, feeding my baby, smelling my baby, and wearing my baby close to me every chance I could because I had to put him down so much to pump out his food. My older kiddos watched way too much TV most of the time. Some nights I would miss then so much that I would hand the baby to my husband so I could cuddle my girls for a few minutes at bedtime. Some days were extra hard when I felt like a terrible mother to my big girls for being so distracted with feeding their brother. I pumped at dance class and in the car and at occupational therapy appointments and in the Target parking lot and in the car pool line at preschool.
When I couldn’t see the progress through all the stress and despair there was my IBCLC, my friends, and my family reminding me of the incremental steps we were making and encouraging me to keep going.
Slowly, slowly, slowly there was progress.
Tensions unwound, muscles strengthened, and a baby grew.
One day in early December I was chatting with my IBCLC and giving her a status update. A few weeks prior I had returned to the pediatric dentist for the buccal release that we suspected was keeping our progress stalled. After that release it seemed that he started making a big jump in feeding ability. Our OT had discharged us from therapy because the torticollis was resolved and he was feeding well on the special needs feeder we had been using moving from the easiest milk flow to the hardest. I had this gut feeling that he was ready to fly solo. I talked over my ideas with my IBCLC and pediatrician and both of them felt like it was time to try.
We made a plan to do a three week trial of exclusive breastfeeding over the Christmas holiday. At the end of the three weeks I would go back to my pediatrician and we would do a weight check to see how he did. I was forbidden from weighing him at home on my scale. I spent spent a few anxiety riddled days mentally preparing for our next and hopefully last hurdle and on a Saturday morning I woke up and breastfed my son.
Afterwards, I didn’t give him a bottle.